Substance Abuse
The United States faces a complex and evolving crisis when it comes to substance use disorders (SUDs). These disorders affect people across demographics. It destroys lives and strains families, communities, and healthcare systems.
Understanding the shocking scale of this problem, along with its risk factors, is crucial for creating prevention and treatment programs that save lives.
- Nearly 50 million Americans experienced a substance use disorder in the past year.
- Despite the widespread need, only a tiny fraction (9.1%) of those with co-occurring mental health issues and SUDs receive treatment for both conditions.
- Over 70% of individuals with alcohol abuse or dependence never receive treatment.
- Suicidal thoughts are alarmingly common, affecting over 13 million US adults and 3.4 million adolescents in the past year.
- Addiction doesn’t discriminate: heroin use has increased across all income levels in recent years.
This article draws on the most recent and reliable data sources available. By focusing on up-to-the-minute information, we gain the clearest possible picture of the challenges and the best ways to address them.
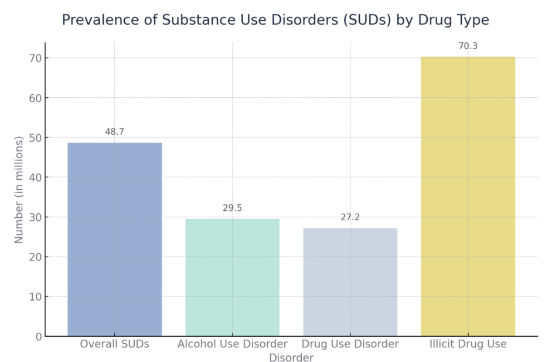
Prevalence of Substance Use Disorders by Drug Type
Substance use disorders (SUDs) affect a significant portion of the US population. In 2022, the numbers reveal the varying prevalence of different substance-related disorders:
Overall Substance Use Disorders
- An estimated 48.7 million Americans aged 12 or older had a substance use disorder (SUD) in the past year.
Alcohol Use Disorder (AUD)
- Alcohol use disorders were the most common, affecting 29.5 million people.
Drug Use Disorder (DUD)
- 27.2 million people had a drug use disorder.
- Of those with DUD, 8.0 million also had an alcohol use disorder, highlighting the overlap between the two.
Illicit Drug Use
- Around 70.3 million people aged 12 or older used illicit drugs in the past year.
- Marijuana was the most common illicit drug, used by 61.9 million people (22.0% of those aged 12+).
Latest addiction statistics 2023 National Survey on Drug Use and Health (NSDUH) – Source: Recovery Team
Excessive Alcohol Use
Excessive alcohol use includes binge drinking, heavy drinking, and any drinking by pregnant women or people younger than the legal drinking age. Binge drinking, the most common form of excessive drinking, is defined as consuming 4 or more drinks during a single occasion (for women), and 5 or more drinks during a single occasion (for men). Although most people who binge drink do not have a severe alcohol use disorder, binge drinking is a harmful risk behavior associated with serious injuries and multiple diseases.
Excessive alcohol use, including binge drinking, is associated with short-term (e.g., alcohol poisoning, overdoses, injuries, violence) and long-term (e.g., liver disease, cancer, heart disease, hypertension) health conditions. Excessive alcohol use increases a person’s chances of engaging in risky sexual activity including unprotected sex, sex with multiple partners, or sex with a partner at risk for sexually transmitted infections (STIs). It is also associated with unintentional injuries (e.g., motor vehicle crashes, falls, burns, alcohol poisoning); violence (e.g., homicide, suicide, intimate partner violence, sexual assault); and STIs.
Tips for drinking less include setting limits, counting drinks, managing triggers (certain people, places, or activities might tempt the traveler to drink more than planned), and being around people who support moderation in or abstinence from drinking. For more details on excessive alcohol use and its effects on health, see Alcohol and Public Health.
Alcohol Use Disorder
Excessive drinking is also associated with an increased risk for alcohol use disorder, a chronic medical condition. Alcoholics Anonymous provides information on meetings occurring domestically and internationally. Suggest travelers use the acronym HALT (Hungry, Angry, Lonely, Tired) to remind them of the triggers for drinking and the need to take appropriate avoidance measures.
Pharmacologic options are available to assist in treating alcohol use disorder, including acamprosate, disulfiram, and naltrexone. Advise travelers taking disulfiram to avoid “alcohol-free” beers because these products can contain ≤0.5% alcohol, enough to produce a reaction. Moreover, it is inadvisable to initiate first-time pharmacologic intervention at the onset of an international trip.
Cannabis
The cannabis plant contains more than 100 compounds (or cannabinoids). Cannabis (marijuana, weed, pot, dope) refers to the dried flowers, leaves, stems, and seeds of the cannabis plant, as well as concentrates, edibles, extracts, tinctures, vape cartridges, and other products that contain Δ-9-tetrahydrocannabinol, the main psychoactive ingredient of the plant. Because cannabinoid use policies vary from country to country, travelers should review the policies and regulations around transport, possession, and use of cannabis or cannabinoids in the countries to which they are traveling and passing through. In many countries, possession and use of cannabis can result in severe criminal penalties, including imprisonment.
Cannabis has been legalized in some US states for medical or nonmedical adult use, and although its use and possession at some airports might be allowed, cannabis remains categorized as a Schedule I substance in the United States and is illegal at the federal level. Cruise lines follow federal law; federal scheduling of cannabis as a Schedule I substance also prohibits use and possession on cruise ships.
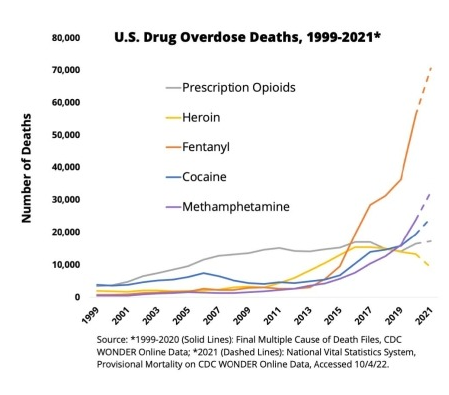
Opioids
According to the National Survey on Drug Use and Health (), in 2020, 9.5 million people aged >12 years reported misusing prescription opioids or using heroin within the past 12 months, and 2.7 million reported having an opioid use disorder (OUD). OUD is not uncommon in the United States, and travel medicine providers likely will encounter patients experiencing, or in recovery for, this condition. Preparing travelers with OUD to travel internationally requires additional planning.
Illicit opioid use and misuse of prescription opioids are factors that increase risk for overdose. Evidence-based strategies for reducing the risk for overdose associated with illicit opioid use include use of fentanyl test strips (FTS) and access to naloxone. FTS are used to determine whether fentanyl has been mixed with drugs; naloxone can reverse an overdose from opioids, including fentanyl, heroin, and prescription opioid medications.
Medications for Treating Opioid Use Disorder
Medications are available to effectively prevent overdose, treat OUD, and sustain recovery; these medications might be restricted or prohibited in other countries, however. Examples of medications used to treat OUD include buprenorphine and methadone, which act as opioid agonists. These medications reduce cravings and withdrawal symptoms and block the effects of other opioids (e.g., heroin). The opioid antagonist naltrexone works by blocking the effects of opioids.
The Transportation Security Administration (TSA), US Department of State, and US Centers for Disease Control and Prevention (CDC) provide guidance for traveling with prescription medications, including medications used to treat substance use disorders. Travelers should check with the US embassy located in the country they plan to visit or travel through to make certain their medications are allowed in that country and determine whether they need any documentation to bring medications. The International Narcotics Control Board provides information on country regulations for travelers carrying medications containing controlled substances.
Travelers should carry all medications in their original labeled container with a copy of the prescription printed on the container and a statement from the medical director of the clinic or prescribing physician on letterhead detailing the care being provided. The name listed on prescriptions, medication bottles, and letters from health care providers should match the name on the traveler’s passport. Although medications can be packed in carry-on or checked baggage, traveling with prescriptions in carry-on luggage can help to ensure ready access to medications in an emergency or if checked luggage is lost.
Methadone
In the United States, methadone treatment programs are strictly regulated by the federal government, and methadone treatment for OUD can only be dispensed by federally certified opioid treatment programs (OTPs); regulations include prerequisites to be eligible for take-home medication. Most methadone treatment programs dispense the medication daily in person, and a patient must complete continuous treatment in an OTP for >12 months before being permitted to take home >1 week’s supply of methadone. A maximum of 1 month’s (31 days) supply of methadone can be provided to patients who have completed 2 years of continuous treatment.
Recovery Support Services
Encourage patients with OUD to review information about recovery support services in other countries, such as information provided on the Narcotics Anonymous website. In addition, global advocacy and support groups are available for people taking methadone and other treatments for OUD. For instance, the German organization INDRO E.V. operates the Coordinating and Information Resource Center for International Travel by Patients Receiving Methadone and other Substitution Treatments for Opiate Addiction and publishes International Travel Regulations for Patients Participating in Drug Substitution Treatment and the Methadone Worldwide Travel Guide.
Substance Use Disorder Treatment
A subtype of “medical tourism” (see Sec. 6, Ch. 4, Medical Tourism) involves travel to another country for SUD treatment and rehabilitation care (“rehab tourism”). Box 3-10 lists some pros and cons of tourism for substance use disorder treatment. Travelers exploring this option might be seeking a greater range of treatment options at less expense than what is available domestically.
Before a traveler selects an international program for SUD treatment, encourage them to review information that can help them better understand proposed treatments. Evidence-based guidance is available from the Substance Abuse and Mental Health Services Administration (Medication Assisted Treatment, Co-Occurring Disorders and Other Health Conditions, Treatment of Stimulant Use Disorders) and CDC (Evidence-Based Strategies).

All information obtained on this page is from the Center for Disease Control and Prevention & Cure Addiction Group.
